Retina Clinic
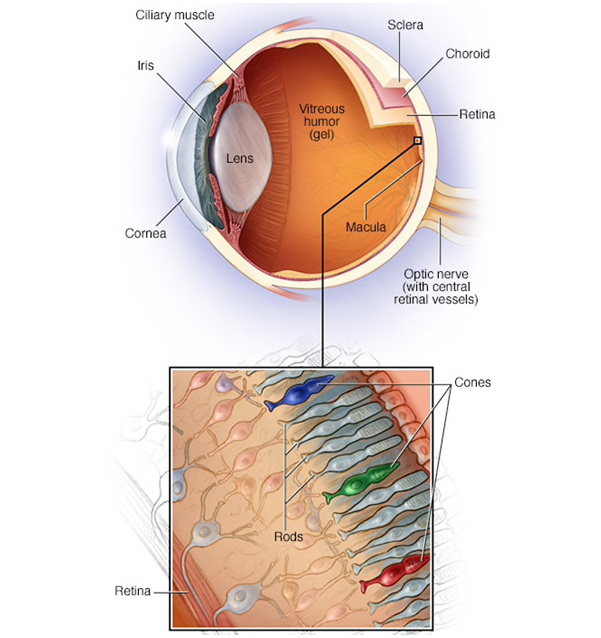
Retina is the layer at the back of the eyeball that contains cells sensitive to light, which trigger nerve impulses that pass via the optic nerve to the brain, where a visual image is formed. It is important to do a retinal examination in the routine eye checkup is because most of the pathology can be picked up early can be treated and prevented from causing blindness.
To examine the retina, an ophthalmologist will dilate, or widen, your eyes during a comprehensive examination using eye drops. A retina specialist then uses a special magnifying lens to exam your retina. The dilation will reverse after several hours.

Warning Signs of Retina Problems
Now that you know how the retina works, let’s look at some of the top symptoms that could indicate you have retinal problems.
1. Flashing Lights
Flashing lights can be a symptom of a number of conditions including migraines, eye injury, and retina problems. If you don’t often suffer from headaches or have never experienced random flashing lights before, this can be a sign that you could have a retinal disease or problem.
As we went over earlier, the retina is responsible for sending light signals to the brain. When the retina is damaged or diseased, it can send incorrect and/or abnormal signals to your brain, which could cause you to experience this “flashing light” phenomenon.
2. “Dimmer” Vision
Dim vision can be characterized as things looking darker than usual, being “muddied”, and seeing less contrast. Some compare it to how it looks when you wear slightly tinted sunglasses or dimming the light switch on an overhead light.
3. Distorted Vision
Distorted vision is the most common complain that a patient with retinal problems experience a few types of distorted vision, including:
• Double vision
• "Wavy" lines
• Things appearing crooked
• Blurred vision
The severity of these vision problems can vary, and many people mistake their blurry vision as simply worsening vision related to age. However, you should always be evaluated by an eye care professional to rule out serious issues like a retinal disease of the the Macula, the most sensitive part of the retina and region of perfect vision
4. Specks and/or Lines in Vision
We’ve all experienced this before you see random dots or lines in your vision for a few minutes before they disappear this is called entoptic phenomenon - caused by white blood cells moving in the capillaries in front of the retina. These are normal and happen to all of us at some point.
5. Blind spot
A small portion of the visual field of each eye that corresponds to the position of the optic disk (also known as the optic nerve head) within the retina. There are no photoreceptors (i.e., rods or cones) in the optic disk, and, therefore, there is no image detection in this area.
Symptom-producing pathological scotoma may be due to a wide range of disease processes, affecting any part of the visual system, including the retina (in particular the macula), the optic nerve and even the visual cortex Even a small scotomathathappens to affect central or macular vision will produce a severe visual disability, whereas a large scotoma in the more peripheral part of a visual field may go unnoticed by the bearer because of the normal reduced optical resolution in the peripheral visual field
Common Retinal Problems
Inherited Retinal Discorders :
Inherited retinal diseases are any retinal diseases that were genetically passed on from a relative. The most common inherited retinal diseases include retinitis pigmentosa and Stargardt’s disease. Patients with Stargardt’s disease, Best’s disease, or pattern dystrophies are evaluated for more serious secondary changes like choroidal neovascularization (the growth of abnormal blood vessels under the retina), and patients with retinitis pigmentosa are monitored for the development of cataracts and macular edema.


Diseases can cause a significant reduction in peripheral and/or central vision that is often slowly progressive and begins at an early age. Since these diseases tend to run in families, the role of genetic counseller and vocational trainer plays vital role. Importance of family screening is vital. The benefits of government aids and self-sustained are to be mentored constantly.
Systemic Disorders in the Eye :
Systemic diseases are diseases that involve many organs or the whole body. Many of these diseases also affect the eyes. In fact, an eye exam sometimes leads to the first diagnosis of a systemic disease.
The most common systemic disease:
- Diabetes mellitus – an imbalance in blood glucose (sugar) levels causes diabetic retinopathy
- Acquired immunodeficiency syndrome (AIDS) – a life-threatening disease caused by a virus that cripples the body’s immune defenses and manifests as uveitis and less commonly can cause infectious diseases like toxoplasma retino-choroiditis, cytommegalo virus retinitis, ocular tuberculosis and herpes zoster ophthalmicus , fungal and even tumour like kaposis sarcoma.
- Graves’ disease – a thyroid disorder, most often in women, which can cause a goiter (swelling in the front part of the neck) and protruding eyes or exophthalmos and is a autoimmune condition where the Immune cells affects the ocular muscles.
- Sarcoidosis – a disease that mainly affects the lungs, brain, joints and eyes, found most often in young African-American women.
- Systemic lupus erythematosus – a connective tissue disorder involving mainly the skin, joints and kidneys and causes severe dry eye scleritis and retinal vasculitis in the eye and requires long term care as patients are on oral Immunousupressives and steroids and are at the risk of developing secondary complications like complicated cataract, glaucoma.
- Rheumatoid Arthritis: an autoimmune disease that affects the eye causing episcleritis, scleritis and a dry eye called kerato-conjuctivitis sicca.
- Hypertension (high blood pressure): is associated with observable changes in the retinal microvasculature, including retinopathy, choroidopathy and optic neuropathy, as well as with an increased risk of ocular vascular abnormalities such as arterial and venous occlusive diseases, retinal macro aneurysm formation and embolic events.
- Atherosclerosis (hardening of the arteries)
- Sickle cell disease – an inherited blood disorder that can block circulation throughout the body, primarily affecting African - Americans.
- Multiple sclerosis – a disease that damages nerve coverings called myelin sheath , causing weakness, coordination and speech disturbances. They can have their presentation with acute defective vision due to retro-bulbar optic neuritis or optic neuritis.
For any of the eye problems mentioned above, it is important to have an examination by an ophthalmologist, who will confer with your primary care physician.
Degenerative Retinal Disorders
Age Related Macular Degeneration:
Macular Degeneration is caused by the deterioration of the central portion of the retina, the inside back layer of the eye that records the images we see and sends them via the optic nerve from the eye to the brain. The retina’s central portion, known as the macula, is responsible for focusing central vision in the eye, and it controls our ability to read, drive a car, recognize faces or colors, and see objects in fine detail.
.png)
There are two basic types of Macular Degeneration: “dry” and “wet.” Approximately 85% to 90% of the cases of Macular Degeneration are the “dry” (atrophic) type, while 10-15% are the “wet” (exudative or neovascular ) type.
Risk factors include:
- Increase in age
- Family h/o AMD
- Smoking
- Poor dietary habits
Myopic Retinal Degeneration:
Myopia (also called nearsightedness) is the most common cause of impaired vision in people under age 40.Myopia occurs when the eyeball is too long, relative to the focusing power of the cornea and lens of the eye. This causes light rays to focus at a point in front of the retina, rather than directly on its surface. Mopia is corrected with good refractive glasses, contact lenses or corrected by refractive laser procedures or implantable -collamelar lenses (ICL) and are controlled by low-dose atropine eye drops in school age children. Pathologic myopia represents a subgroup of myopia and affects up to 3% of the world population.High myopia or pathological myopia is defined as refractive error of at least -6.00D or an axial length of 26.5mm or more.


Pathophysiology of Myopia :
The main factors proposed for driving the development of pathologic myopia are elongation of the axial length and posterior staphyloma. Biomechanical forces related to axial elongation of the eye result in stretching of the ocular layers and progressive thinning of the retina, choroid and sclera.
This emphasises the need for a thorough macular examination with retinal peripheral depressed examination as a part of routine yearly checkup, to prevent serious complication like retinal detachment. In particular, lacquer cracks, myopic schisis, or choroidal neovascularization in the macula area and holes or tears in the periphery of the retina should be routinely screened and patient education of these conditions to be discusses with patients and family members.
Retina Clinic
Dr. Padma M.B.B.S, M.S.
